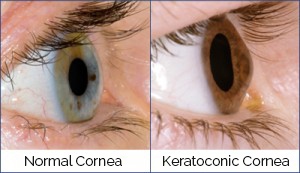
Keratoconus (ker-uh-toe-KOH-nus) occurs when your cornea — the clear, dome-shaped front surface of your eye — thins and gradually bulges outward into a cone shape.
The cornea is the window of the eye. Light travels through the cornea past the lens to the retina and then the brain to form a visual image. The normal corneal surface is smooth and aspheric i.e. round in the center, flattening towards its outer edges. Light rays passing through it moves in an undistorted manner to the retina to project a clear image to the brain. A cone-shaped cornea causes blurred vision and may cause sensitivity to light and glare.
Keratoconus usually affects both eyes and generally occurs in people ages 10 to 25. In patients with keratoconus the cornea is not only cone shaped but the surface is also irregular resulting in a distorted image being projected onto the brain. The condition may progress slowly for 10 years or longer. Keratoconus typically commences at puberty and progresses to the mid-thirties at which time progression slows and often stops. Between age 12 and 35 it can arrest or progress at any time and there is no way to predict how fast it will progress or if it will progress at all. In general, young patients with advanced disease are more likely to progress to the point where they may ultimately require some form of surgical intervention.
Many patients are initially unaware they have keratoconus and see their eye doctor because of increasing spectacle blur or progressive changes in their prescription. Keratoconus is most often diagnosed by a cornea specialist who may see typical findings when examining the patient.
Because the cornea is irregular and cone shaped, glasses do not adequately correct the vision in patients with keratoconus since they cannot conform to the shape of the eye. Vision problems can be corrected with glasses or soft contact lenses early on in the condition. As keratoconus progresses, you may have to be fitted with rigid gas permeable contact lenses or other types of contact lenses. Advanced keratoconus may require a cornea transplant. Patients with keratoconus see best with rigid contact lenses since these lenses provide a clear surface in front of the cornea allowing the light rays to be projected clearly to the retina. Hence the vast majority of patients are treated with rigid contact lenses.
Corneal Cross-Linking
In patients with keratoconus, the cornea can become weak, thin, and irregularly shaped. The corneal cross-linking procedure adds stable cross-links to the cornea, preventing the cone shape, and strengthening the focusing power. This will ultimately stop the thinning process of the cornea, as well as additional loss of vision.
